Why Doesn’t Insurance Cover Spinal Decompression?
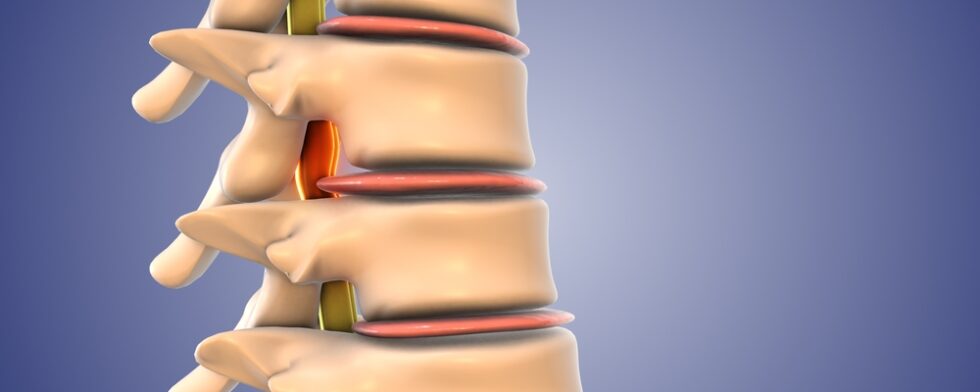
Spinal decompression therapy is a non-surgical treatment designed to relieve pressure on spinal discs and nerves. Many patients hope insurance will cover the cost, but coverage is often limited. Understanding the reasons can help patients plan for treatment expenses.
Classification As Experimental
Insurance companies commonly classify non-surgical spinal decompression as experimental or investigational. This classification is based on…
- Limited high-quality clinical research demonstrating consistent long-term outcomes
- Variability in patient responses to decompression therapy
- Differences in techniques and devices used across clinics
Because insurers prioritize treatments with strong evidence of effectiveness, non-surgical decompression often falls outside standard coverage policies.
Medical Necessity Requirements
Insurance plans generally cover treatments deemed medically necessary. While spinal decompression may relieve symptoms, many insurers consider it optional or adjunctive. Coverage is more likely when…
- Other conservative therapies, such as physical therapy, have failed
- Clinical documentation clearly shows nerve compression or disc injury
- Decompression is part of a broader, physician-approved treatment plan
Even then, insurers may limit benefits or deny coverage if they determine the procedure lacks sufficient evidence.
Billing & Coding Challenges
Coverage can also be affected by how the procedure is billed.
- Some clinics bill spinal decompression under general traction or therapy codes
- Incorrect or non-standard codes may trigger insurance denial
- Documentation must demonstrate the medical necessity of each session
Proper coding and documentation can increase the chances of partial reimbursement, but full coverage is rare.
Variability Across Insurance Plans
Private insurance, Medicare, and Medicaid each have different rules.
- Most private plans exclude non-surgical decompression
- Original Medicare generally does not cover it due to its experimental status
- Some Medicare Advantage plans may provide limited coverage under certain therapy codes
- Workers’ compensation or auto insurance may cover it if it is part of injury rehabilitation
Coverage depends heavily on the specific plan, state regulations, and prior authorization requirements.
Out Of Pocket & Alternative Options
Since insurance often does not cover spinal decompression, patients frequently pay out of pocket. Clinics may offer…
- Package pricing for multiple sessions
- Payment plans to spread costs
- Discounts for cash payments or bundled care with physical therapy
- Use of health savings accounts or flexible spending accounts if the treatment is medically necessary
Insurance often does not cover spinal decompression because it is classified as experimental, evidence of long-term effectiveness is limited, and coding can be complex. While partial reimbursement may be possible under certain conditions, most patients pay out of pocket. Understanding these limitations helps in planning treatment and exploring alternative payment options.
